Please note that a more recent article on Suicide statistics and strategy in Northern Ireland: Update was published in November 2019.
______________________________
For the second consecutive year, Northern Ireland recorded the UK’s highest suicide rate. Provisional figures for 2015 show a figure of 318 recorded deaths by suicide in Northern Ireland. This compares with a total of 268 for 2014. In recent years, suicide rates have increased substantially from their typical level in the 1970s. For example, in 1971 a suicide rate of 5 per 100,000 population was recorded, and the rate remained in single figures for most of the next thirty years [1]. In the last decade, however, the rate has fluctuated around the mid-teens (14-17 per 100,000 population). There are many reasons why someone may experience suicidal feelings, and suicide is a highly complex issue. So what are some of the risk factors?
Deprivation
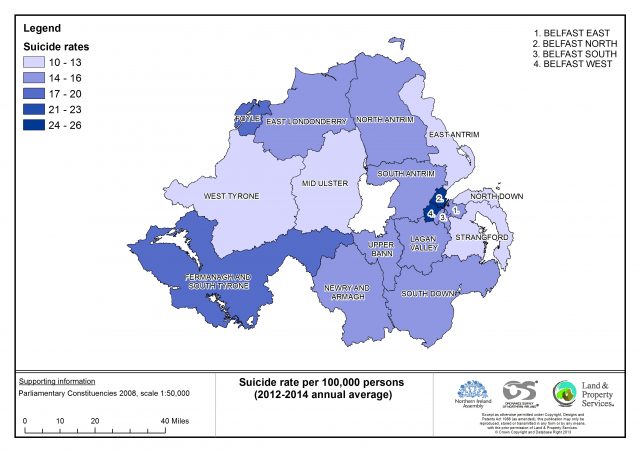
Suicide and deprivation are closely linked. Belfast North and Belfast West are the two constituencies with the highest average annual suicide rate. The Northern Ireland Multiple Deprivation Measure 2010 found these to be the two most deprived constituencies.
Self-harm
The rate of self-harm hospital admissions is four times higher in the most deprived areas than in the least deprived areas.
Between April 2013 and March 2014 there were 8,453 presentations at hospital emergency departments in Northern Ireland as a result of self-harm, involving almost 6,000 people. A further 3,623 cases attended emergency departments with suicidal ideation.
A recent Ulster University study commissioned by the Public Health Agency reviewed over 1,660 records of suicide and probable suicide from the Northern Ireland Coroner’s database. It found that around half of the deceased had made previous suicide attempts or had a record of suicidal thoughts.
Gender
In Northern Ireland, men are three times more likely to die by suicide than women. This has been partly attributed to differences in methods used, as men tend to use more lethal methods such as hanging. Cultural perceptions of masculinity, which define men as competitive and strong, are also thought to impact negatively upon help-seeking behaviours in men.
Employment status
Unemployment is another potential factor contributing to suicide, particularly for younger age groups and men. Data from the recent coroner’s database study showed that at least half of the deceased were known to be unemployed.
Alcohol and substance use
The misuse of substances is closely linked with self-harming and suicide. Dependent substance misusers are more likely to display other major risk factors.
Alcohol is a key area of concern. For example, The Adult Drinking Pattern Survey (2013) reported that while 73% of adults in Northern Ireland drank alcohol, 31% engaged in at least one weekly binge drinking session and 11% were identified as problem drinkers.
Bereavement
Research has shown that more than one in ten of those who died by suicide reported events relating to experiences of death, grief or illness of, among others, spouse, family members and partners.
Bereavement due to suicide is also associated with increased depression and risk of suicide. Furthermore, there is also a ‘ripple effect’ for families and communities, with up to 60 people being affected by each death.
Legacy of conflict
Research has also shown that ‘the Troubles’ may be a key factor in rising suicide rates. For example, children caught up in difficult or violent situations may be less ‘psychologically resilient’ in later life. This risk factor has not been addressed in current suicide prevention strategies.
Prevention
Effective suicide prevention relies on identifying factors involved in vulnerability and providing opportunities for intervention. Stigma is a major barrier to seeking help. Despite the wide range of suicide prevention services available, many of those who die are not known to health and social care services beforehand.
Prevention is not just a health matter, as suicide is a behavioural outcome which results from a combination of social, psychological, and biological processes, together with the ability to carry out the act.
The existing Protect Life Strategy (2012-2014) dates from 2012. In this new mandate, the Department of Health has just launched a consultation on Protect Life 2 – A Strategy for Suicide Prevention in the north of Ireland with the intention of reducing the overall suicide rate, and more specifically reducing the differential in the suicide rate between the most deprived areas and the least deprived areas.
[1] The suicide rate (per 100,000) rose above single figures in only five years between 1971 and 2001.