This is the second in a series of articles regarding mental health and illness in Northern Ireland. Recently, we provided an overview of mental health strategy in Northern Ireland; here, we focus on service delivery for adults, for children and adolescents, and the importance of the ‘recovery’ focus of the model of care. A more detailed RaISe briefing on many of the issues is available.
Patient Journey – Overview
The first ‘step’ for an individual is usually a visit to their GP who will assess the person’s needs and determine the best course of action with them. The GP may treat them directly or refer them to mental health services within the Health and Social Care (HSC) Trusts. If a referral is made, mental health services will determine the level of priority and contact the person to make an appointment. When referred to mental health services, a psychiatrist, psychologist, social worker or a mental health nurse may assess the person and ask about:
- Current problems, thoughts and feelings;
- Personal history, including any previous mental health problems and treatments;
- Social history, including details about relationships, family life and lifestyle; and,
- Physical health needs, including any medication taken.
Mental health services will explain any diagnosis and will work with the person to develop a personal well-being plan, summarising their needs and bringing together treatment and care options to help recovery. The types of services that this may cover includes:
- Primary care talking therapies teams: support by counsellors or well-being coaches;
- Community mental health services: care provided by HSC Trusts by one or more of – nurses; social workers; psychiatrists; psychologists; occupational therapists; family therapists; and psychotherapists;
- Acute mental health services: care provided by HSC Trust Crisis Resolution and Home Treatment Teams or specialist hospital care team; and,
- Specialist services: care from a specialist team e.g. alcohol or drug addiction; eating disorders; and personality disorders.
The standards of care are set out in the Service Framework for Mental Health and Wellbeing (2012), underpinned by the ethos of ‘recovery’ and with 58 standards. Service Frameworks for health set out standards of care that patients, clients, carers and wider family can expect, both in a generic sense and specific to the particular health area, as informed by expert advice and by national standard setting bodies.
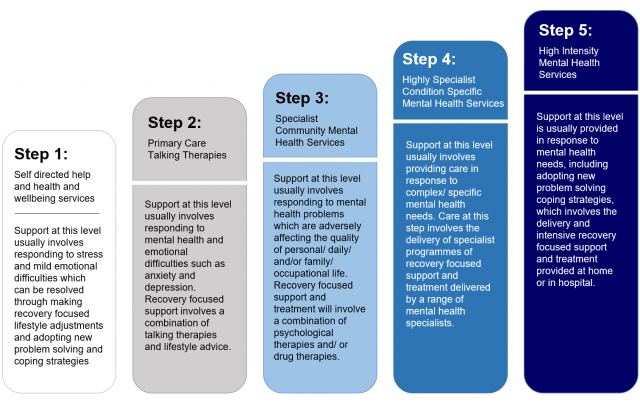
The Stepped Care Model – Adults
The Stepped Care model for regional mental health service provision was first proposed for NI by the Bamford Review (as advocated by the National Institute for Health and Care Excellence (NICE) for common mental health conditions).
The Bamford Action Plan 2009-11 highlighted that the model would provide the framework for all future commissioning and delivery of mental health services, with the number and nature of steps varying to address needs. The steps progress from awareness, recognition and assessment/ diagnosis, within primary care at Step 1, through to the highest steps of inpatient or intensive treatment programmes.
In 2014, the Health and Social Care Board (HSCB) and Public Health Agency (PHA) published a regional mental health care pathway for adults, You in Mind, which was jointly developed by ‘experts by experience’ and professionals. Its purpose is to provide guidance on the steps of care and enhance quality of service and consistency across NI – ‘stepping up’ to intensive/specialist services and ‘stepping down’ depending on the individual’s needs.
The Stepped Care Model – Children and Adolescents (CAMHS)
In 2011, a Review of CAMHS in NI was published by the Regulation and Quality Improvement Authority (RQIA), including the progress of recommendations from the Bamford Independent Review of CAMHS (2006). The review team found a committed workforce and that progress had been made, including the inpatient unit (Beechcroft) and services such as eating disorders and crisis intervention. However, the RQIA concluded that more work was needed and made recommendations for the organisation and delivery of CAMHS.
As a result, the HSCB developed a stepped care model for children and young people with developmental, emotional and mental health needs. Since then HSC Trusts have been aligning their services with this model.
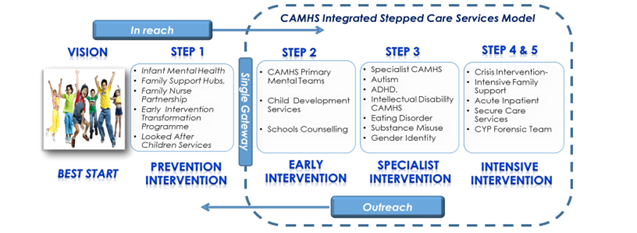
An Integrated Care Pathway for CAMHS is also in development to set out service standards across the steps and is being co-produced with parents, young people and voluntary sector organisations. A range of other support for the stepped care model has been developed. The HSCB in partnership with Trusts, children and young people has produced a regional guide to CAMHS Services called ‘Mind Matters – A Guide to Child and Adolescent Mental Health Services’.
With regard to early intervention, the HSCB have developed Primary Mental Health Step 2 Care Teams with teams who are now operating across NI and the PHA has recently published an infant mental health plan. Across NI there are 29 multi-agency Family Support Hubs, with a Primary Mental Health Worker linked to each Hub to promote earlier access to services.
The HSCB developed the Family Support NI website which includes CAMHS information and HSC Trusts have developed their websites to improve information and are strengthening advocacy services.
In 2016, the HSCB completed a three year review of the CAMHS Stepped Care Model, which included a summary of the progress being made by all HSC Trusts against agreed quality (implementation) indicators.
Recovery
The Bamford Review Strategic Framework for Adult Mental Health Services (2005) established the focus of service planning and provision on the concept of ‘recovery’, with the recommendation that:
A person-centred approach to service planning and provision must be adopted with recovery core to the vision of strategic development.
It is thought that the concept of recovery from mental illness had its inception with deinstitutionalisation in the 1960s and 70s. During the 1980s community support systems combined with rehabilitation laid the foundation for the vision in the 1990s of the promotion of wider ‘recovery’ from mental illness[1]:
People with mental illness may have to recover from the stigma they have incorporated into their very being; from the iatrogenic effects of treatment settings; from lack of recent opportunities for self-determination; from the negative side effects of unemployment; and from crushed dreams.
Around 2008-09 ‘recovery’ from mental illness became a key UK government objective and organisational challenges for implementing recovery were identified, including increasing ‘personalisation’ and choice; ensuring organisational commitment; establishing ‘Recovery Education Centres’; and increasing opportunities for building a life ‘beyond illness’.
A three-year project, ImROC (Implementing Recovery through Organisational Change), ran in England from 2009 with 29 sites. It delivered joint training sessions (‘co-produced’ between staff and service users) to more than 400 staff, service users and managers; supported recruitment and training for over 150 Peer Support Workers to work as peer trainers; and established six Recovery Colleges. The key service developments were Recovery Colleges and Peer Support Workers.
In NI, Recovery Colleges are now established in each HSC Trust offering courses on topics around mental health designed to be of interest to service users, carers, families, and professionals. In October 2016, the former Health Minister, Michelle O’Neill, welcomed the launch of the latest Recovery College in the Southern HSC Trust and also Wellmind Hubs.
The Hubs offer a range of support options for people with common mental health conditions such as anxiety, stress or low mood. Care is offered by independent sector providers, community groups or from within the Hub. The Hubs have been initially set up in the Armagh and Dungannon areas and plans are underway to extend them into the Craigavon/Banbridge and Newry/Mourne localities.
The Care Pathways and Stepped Care Models in NI are built around the premise that access to treatment and care needs to be personalised and ‘recovery’ orientated. Drawing on the experiences and skills of people who use mental health services and those who work in them, enabled the development of the above-mentioned ‘You in Mind Mental Health Care Pathway’, which redefined how services are delivered to create an environment that supports recovery. The aim is a focus on the service user and professionals working together as equals to determine a path to recovery.
[1] Anthony William A. (1993) ‘Recovery from mental Illness: The Guiding Vision of the Mental Health Service System in the 1990s’, Psychosocial Rehabilitation Journal, 16(4), 11-23.

