This is the third in a series of articles on mental health and illness in Northern Ireland. Following posts on the overall strategies for mental health and care pathways, this article focuses on barriers to accessing mental health services and highlights the role of the voluntary sector in delivering such services. A more detailed RaISe briefing on many of the issues is available.
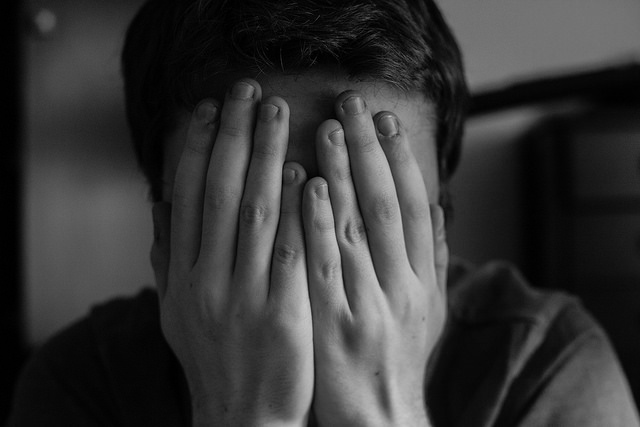
Stigma – a key barrier to accessing help
The World Health Organisation (WHO) states that the most important barrier to overcome in the community is stigma and discrimination towards people with mental health and behavioural disorders. The discord between a person’s self-perception and common stereotypes about mental illness cause people to avoid telling others about their mental illness and leave many masking the symptoms. Together with anticipated or experienced negative consequences, they are deterred from seeking help.
Given the high rates of suicide and self-harm in NI, understanding why people do not seek help and the barriers they face in accessing help is imperative. A recent RaISE briefing provided the disturbing information that suicide rates in NI were the highest in the UK for a second consecutive year and that 72% of those who died by suicide in NI did not have any contact with mental health services.
It is known that between 40% and 60% of those who die by suicide have a history of self-harm. There were 25,620 self-harm presentations at emergency departments in NI in a three year period involving 16,301 individuals. More than a third (36%) of these were as a result of repeat acts, with one in five re-presenting within 12 months of their first attendance. Repeat self-harm is most likely to be associated with self-cutting, yet many of these patients are discharged following treatment, or leave without being seen.
Research suggests that several types of stigma deter a person from seeking help for mental health issues. These include:
- Anticipated and/or experienced stigma of being treated unfairly;
- Internalised stigma when holding stigmatising views about oneself;
- Perceived stigma about the extent to which people, in general, have stigmatising attitudes/behaviour towards people with mental illness;
- Stigma endorsement which is the person’s own stigmatising attitudes/behaviour towards people with mental illness; and,
- Treatment stigma associated with seeking or receiving treatment for mental ill health.
Internalised and treatment stigma were found to have a consistent negative association with seeking help. It is therefore recommended that anti-stigma programmes should focus on countering stereotypes that view mental illness as a ‘weakness’. Those already receiving treatment should be supported in developing additional strategies to cope with and counter internalised and treatment stigma. Services that minimise a stigmatising effect are those that avoid unnecessary labelling, respect confidentiality, and are community based.
Voluntary sector services
The Evaluation of the Bamford Action Plan 2009-2011 recognised the important role of the voluntary and community sector in the delivery of mental health services in the community. This has also been recognised by professionals, service users, and carers, with a mental health professional in the voluntary sector stating that:
[A] positive trend at the moment is the increase in availability of therapeutic type services that are community-based, delivered through the voluntary sector, and more accessible to people who are not necessarily in the care of a psychiatrist …accessed directly.
Research evidence
A Northern Ireland study of suicidal young men found that formal mental health services by their ‘type, nature, and geographical location’ offered only limited help for young men with suicidal thoughts and behaviours. Services that were more pro-active, including outreach services and ‘drop-in’ suicide centres were valued as these were in line with their preferred ways to interact socially. Being part of a peer group was important, with the opportunity to discuss issues in a safe forum with others who had similar thoughts and feelings. Being exposed to those who were no longer suicidal offered the chance to see that recovery was possible. Mental health professionals had a role in replacing perceptions of what a ‘successful’ man should have attained with achievable goals.
Research reflects support for services delivered by the voluntary sector. Learning life skills, social skills and taking part in educational programmes have been found to be useful in navigating contemporary life challenges. It is recommended that mental health services should be embedded in non-mental health environments such as sports clubs, schools, the workplace and community interest and self-help groups. There is also an acknowledgement that support needs to be available over the long term as there is no ‘quick fix’ to mental health issues. Suicide related services need to reach out to young men pro-actively and these should be community based, open access, and widely publicised.
In relation to services, the research recommended that psychological therapies should be available as part of routine care. In 2015, in response to the use of prescription drugs for anxiety and depression being higher than elsewhere in the UK, Mental Health Hubs were introduced in each of the five NI Local Commissioning Group areas. The aim is to provide GPs with alternatives to long-term medication for common mental health issues and to promote prevention and early intervention with an all-inclusive approach from a variety of providers. These can include counselling, cognitive behavioural therapy (CBT), group therapy, facilitated self-help, life coaching, signposting to other support services, and support for linking into the community and social activities.
Some examples from Northern Ireland of voluntary sector delivery
In Northern Ireland, the community and voluntary sector currently deliver the Self-Harm Intervention Programme (SHIP) across each of the five Health and Social Care Trust areas. SHIP was established in October 2015 for people who have self-harmed and their carers, and is funded by the Public Health Agency (PHA). The programme originated in the Republic of Ireland (RoI), and an evaluation in 2015 found that its clients benefitted from an increase in wellbeing, including optimism, emotional stability and problem solving skills that included seeking help when it was needed.
Together for You (TFY) was a voluntary sector led project involving nine leading NI mental health charities. It was funded by the Big Lottery Fund from 2013-2016. TFY delivered a range of mental health and wellbeing services across NI, with a key element being to increase understanding of mental health issues and improve the ability of beneficiaries to identify signs of poor mental health. Of the 52,587 beneficiaries of the project, over 90% reported an improvement in their mental health, feeling better able to seek help in relation to their mental health, and being able to direct others to sources of support. A majority of participants (86%) also stated that they would not have received the support they did elsewhere, and the project was found to have exceeded its target both for numbers of beneficiaries and cost efficiency.
Resources – a key issue
A report on mental health services in NI acknowledges that funding cutbacks have impacted on progress in implementing recommendations in the Bamford Review. A recent review of mental health services found that despite a higher level of need, per capita spend on mental health and learning disability in Northern Ireland was less than half of the spend in England.
Adequate resources are required if the voluntary and community sector are to have an impact on mental health services here. The Scottish Government has recognised the need for adequate resources, announcing in 2016 (along with ‘Comic Relief’) an investment of £4.5 million in a three-year anti-stigma and discrimination national programme delivered by the Scottish Association for Mental Health and the Mental Health Foundation. The programme is based on the Scottish Government’s 2002 ‘See Me’ national campaign to address negative attitudes to mental health issues. An evaluation of ‘See Me’ in 2009 found that aspects of the campaign that supported developments at local level were perceived to have been limited by funding constraints. Addressing this, a strategic review published in 2013 highlighted the benefits of the campaign that included long-term (multi-year) government funding and delivery through the voluntary sector. These elements were described as ‘…what were at the time of its creation recognised as key factors for success’.